This blog is no longer active, you can find my new stuff at: george3d6.com, epistem.ink, ontologi.cc, and phenomenologi.cc
Navigating the swamps of medical uncertainty, a personal anecdote
In general, I’ve been skeptical of medicine and medical science.
I’m not skeptical about the scientific method as a whole, or about the ability to apply scientific findings and rational thought to solve medical issues. This seems “obviously” true.
I am simply skeptical that the system we have in place does anything remotely resembling “applying rational thoughts and scientific empiricism to address medical issues”.
I understand many people don’t share my concern, and often just do what their doctor tells them or ignore medicine entirely. But I think that there are some that don’t, which believe that there is truth to be found in medical science, but taking the advice of any random doctor about any random issue is unhealthy.
It is in part for the potential benefit of those people that I want to share my own recent first encounter with a serious medical issue, and my success as well as failure in treating it. I don’t believe what I did was necessarily correct, and this account is greatly simplified, so take it with a grain of salt, as a thriller about navigating the swamps of uncertainty, rather than medical advice.
i - Injury and surgery
It all started on the 30th of July (2021), when, at the age of 25, I seemingly badly injured my knee while swimming in the ocean. My leg was almost unable to move, was in pain, and was swollen. I used topical NSAIDs (likely a mistake) and I went from being barely able to take a few steps unassisted to running up hundreds of stairs in about a week.
A few days after the injury I consulted a doctor, which suggested it may be a meniscus tear, that I should get an MRI and consider surgery if it didn’t get better. Given my rapid healing, I promptly ignored his advice.
A month later, on August 28th, I managed to re-injure said knee, while sitting cross-legged. A weird sleeping position made the pain worse, and that started a month-long quest to find out what’s wrong and whether or not it can be cured.
My first pit-stop on this journey was an Istanbul-based orthopedic surgeon. He worked at an internationally acclaimed hospital, seemed old, wise, and well-spoken, had a fairly impressive h-index, and charged rather “western” amounts for his services.
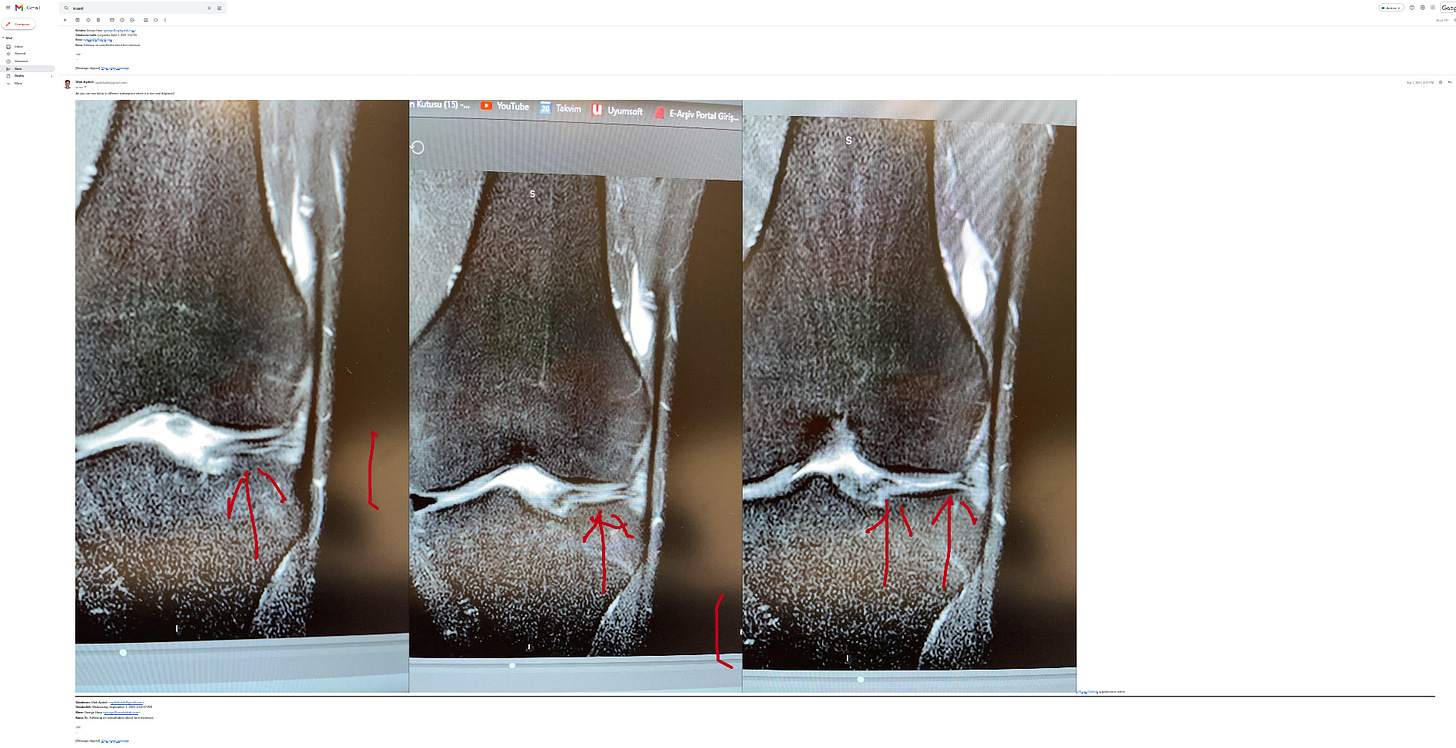
After an MRI he confirmed the diagnosis of a lateral meniscus tear and recommended arthroscopic surgery to either remove part of the meniscus or sew it back together based on what would be observed.
He mentioned the surgery is very common, risks of complications extremely small. For him, it was obviously the best way forward given the diagnosis and the inability of such an injury to heal unaided. The surgery consisted of arthroscopy, to get cameras and tools inside the knee, and then either trying to repair the fault or remove part of the meniscus (or a combination of both).
This is where my slight skepticism came in, and I took a day to think about it and search through the literature. More than a dozen hours in what I found was... disheartening.
The first question to ask is “how likely is it that this guy is right?”, a single study [0] came to my aid. The long and short of it is well summarized by the authors:
The overall accuracy for the clinical diagnosis of meniscal tear was 80.7% and the corresponding accuracy for MRI was 73.7%. Surgical pathology was found in all knees at arthroscopy.
The study was n=57 and 46 of the patients actually had a meniscus injury.
What I cared about was a clinical error, which was made in 11 cases. Given the inherent selection bias here, towards more difficult cases (as observed based on diagnosis), older age, and the patients all accepting to undergo arthroscopy... this didn’t look good.
Arthroscopy is one of those “harmless” procedures, but harmless in terms of surgeon talk, where 5-year mortality doesn’t differ significantly, it’s still inserting 3 metal tubes into the knee and capsule and can cause significant harm [1]. My chance of this being done for nothing is 20% based on this study, but given my age and lack of symptomatic severity, it’s likely much higher. Still, I assume I have a top surgeon, so maybe the outcome is better, and he seems fairly certain. So I proceeded to look through the literature on how effective the actual surgery is, after all, if it doesn’t work there’s no point in doing it.
ii - Preliminary Research
I dug through over 50 papers at the time, and to my utmost surprise, I could find almost no results that attested to meniscus surgery of any sort (partial removal, complete removal, or any type of repair) being superior to conservative treatment or mock surgery (placebo). The results that did find advantages were solely for repair and they were by far the least powered and observed mild differences in pain scores, rather than healing. Given that I didn’t know the type of repair (some had way worse outcomes) or the type of injury, or had any certainty repair was possible, things didn’t look good.
The ones I want to point out are [2] a study (RCT with placebo) that finds no significant difference between surgery and placebo surgery, but there seems to be a non-significant improvement in the placebo group over the surgery group. It is tiny but well ran and the only RCT with placebo, which for surgery is the gold standard, double-blind is impossible.
This study [3] seems to indicate that injury size is a good prognosis for surgery being “required”. This is a good example of what I’ve found in many studies and the implicit assumptions that people end up “needing” surgery at some point, presumably due to chronic unbearable pain or reduced mobility. It also seems to indicate that I can base my decision of how conservative to be based on some characteristics of the injury.
There is an interesting “study” [4] that provides rather promising numbers for meniscus + ACL injury healing conservatively based on an arthroscopic examination after 3 months. The only problem is that it’s... not a study, it’s an abstract, I can’t find anything more complete anywhere, sci-hub included. And it’s from the 90s.
There is an incomplete Cochren review on the subject, I managed to speak with one of the authors, which informed me that it was stopped due to administrative delays and similar reviews coming out during that time, so my most trustworthy source was gone, never to be finished.
There’s a lot of analysis and meta-analysis on the subject. With a few glaring issues:
It is unclear what is happening during the studied surgeries, and indeed, doctors I spoke with seem to basically agree that part of it is “open it up, see how it looks like, do whatever seems to work given the constraints”, which might range from removing the whole meniscus to removing a part, to remove a bit in order to sew the rest together, and “sew the rest together” really refers to a bunch of repair techniques, not to mention artificial scaffolds and such
Most studies are done in older populations, most with degenerative issues, most with conditions that seem much worse than mine... instability, knee locking, issues running or even walking.
A good selection would be [5], [6], [7], all showing similar to unfavorable outcomes for surgery, except for [7] which finds favorable outcomes 6 months afterward, but not later. Then there are studies like [8] and [9], which find small positive effects for repair.
In all cases, both for and against surgery of any kind, I am amazed by the fact that the samples in the studies are very tiny, the nature of the injury is very non-specific, the cases usually look much worse than mine in terms of symptoms, the cause or state of nearby tissue is not specified (although acute vs degenerative should matter a lot).
iii - Changing doctors
What’s next? Well, email the doctor and ask for specifics. Can he classify the type of meniscal tear I have? Does he think it’s acute or might it be degenerative damage with bouts of acute episodes? What type of reconstructive surgery is he likely to use?
I got back a comical case of “mad doctor” for asking the questions, it consisted of the phrase:
I am more than happy to answer your questions. I hope you dont ask either the pilots or taxi driver when you take plain or taxi.
And the following photos of a computer screen:
.. that was it.
This was sufficient to make me decide that, if I did want to get surgery, I should probably find a better doctor.
iv - Digging deeper
In the following months, I did 2 more MRIs to monitor the progress and contacted what must have been at least 30 or so doctors from various walks of life asking if they’d be able to hear out my symptoms and potentially look at some MRIs (paid work, of course, although some outright refused any payment).
Meanwhile, I broadened my horizons, I tried to scour everything on google scholar and looked into the outcome of “novel” treatments. The most promising for mild cases seemed to be PRP [10] and MSC [11] [12] [13] injections. The issue with PRP was that most promising studies combined it with surgery. The issue with MSC was small studies, huge variations in methodology and definitions, nothing specific for the type of injury I assumed I had (meniscus related).
I also found a guy named Ilya, which had a similar issue to myself (acute meniscus injury when young resulting in pain and reduced mobility episodes from some movements), who had hired a researcher to look into the issue for him. Said specialists had come to the same conclusions I was starting to draw by this point. (Shout out to Alexey for introducing us, and shout out to him for helping me out by sharing his time and hard-earned research all while refusing any form of compensation)
I ended up having chats with:
A potentially insane doctor(?)(s?) that has some interesting ideas and a blog I sometimes skim, they (expectedly) recommended I wait and don’t trust any orthopedic surgeon I counter.
An orthopedic surgeon from a German clinic that did bone marrow aspirate treatments as well as surgery for such issues. He opined that the MRI is uninterpretable and to have any hope of finding a root cause I’d need a contrast MRI. His best guess without one was that any pain I felt was caused by an ejected piece of the meniscus floating around, not fully reabsorbed, but he assigned low certainty to this theory.
An orthopedic surgeon from Russia, with which I had a rather awkward chat, using a translator, which by the end of it seemed confused about finding any potential issues in the MRI and (seemingly?) confused that I was worried about this given that it caused me no pain for the moment.
Two doctors (one anesthesiologist, one orthopedist) from clinics focused on “regenerative” therapies which both opined that PRP might help and that, provided no obvious structural damage on the MRI, things like stem cells probably wouldn’t. They both mentioned that if an injury does exist, it’s more likely tendons.
An experienced yoga teacher, becaurse I wanted to keep your horizons wide and I assumed he must have encountered exercise-related knee injuries before. Who recommended isometrics exercise and taking it slow with the leg for at least 2 years.
A radiologist from the hospital I took the MRIs at; he found nothing.
I did speak with a bunch of other people but the conversations were less conclusive in those cases.
Basically, nobody agreed about anything. What’s the root cause? The lateral meniscus, but maybe the medial, but maybe ACL, but maybe a ligament, but maybe a combination, but maybe it’s impossible to tell without arthroscopy, and maybe even with. What causes the pain? Impossible to tell, something something inflammation, the meniscus damaging nearby tissues, tissue compression from meniscus movement, a damaged tendon. What’s the most likely solution? Surgery, wait a few weeks, wait a few months, wait a few years, no idea, not much to do, further investigations, physical therapy, PRP, avoid all movements, bone marrow aspirate.
In the meanwhile, I also looked into exercise regimes and the opinions of physical therapists.
All physical therapists I read seemed to be of the opinion that surgery is never the answer sans situations when you are in extreme pain and nothing else works.
This is the one situation where my life prior to the injury helped me a lot. Back when I was much dumber about my exercise I ended up with loads of odd forms of pain and muscle tightness. In the process of solving these, I found a bunch of really good physical therapists online.
So at least I had one data point about these people. I could trust their opinion mildly more because their method had helped me out before. Still, a therapist recommending conservative treatment with exercise has the same bias as a surgeon recommending surgery.
But problem-specific physical therapy for the knee seems limited to “just go through a standard range of easy exercises without causing much pain”. The methods that were more focused on athletes, for quick and full recovery when your body is still young, seemed heavily contested.
The most widely agreed-upon method I could find was that of the knee over toes guy, which might be the most universally praised fitness channel I’ve ever encountered. I searched criticism of him for hours and found nothing but praise and a few people claiming his method was not that great, but still ok.
I did engage in his routines with relative consistency over the last 3 months and I have noticed increased mobility in various areas. As a smaller anecdote, even sit-ups used to cause me knee discomfort before, and deadlifts sometimes bordered on pain. Recently though, I did a high amount of deadlift reps with ~70kg (which before would have caused me pain) and my knees seemed perfectly fine. That plus the fact that I’ve developed muscles in weird places on my legs and feel myself contract differently when walking makes me think he may be onto something.
One thing I did learn from all of this is that the mechanisms of how a knee work seems to be much more poorly understood than I imagined.
I had some very specific symptoms: everything is fine except for when I sit cross-legged at a tight angle or when I am already in pain and sleep with my leg straightened out flat on my back.
I had multiple good-quality MRIs, two by the same technician.
I had doctors with the ability to examine my leg live, move it, palpate it, ask me about it.
None of them could postulate a likely mechanism for the occasional pain and immobility I had.
Even the two guys that said it was a meniscus tear weren’t sure or able to explain what caused the actual pain or immobility, besides hand waving at “meniscus moves around and causes slight damage and/or inflammatory responses”.
v - Where I’m at
Something in my knee makes it so that, occasionally, when I bend my leg in a certain way, I get pain. I have no idea what it is and I doubt I can find out what it is without getting an arthroscopy, though even with that I might not find out. Of course, even if I had an arthroscopy, it would be a 1-person opinion, and given the huge variability I’ve seen thus far, it wouldn’t help me one bit.
I ended up doing a course of PRP, since I found a clinic that had a take on it I really liked, where it could be done by an experienced anesthesiologist with a very narrow needle, resulting in close to no tissue damage. My leg was back to normal after 2 days, but since then I still got mild symptoms thrice, so it hasn’t been a magic cure.
I started a knee exercise routine, which given my gigantic size, flat feet, and tendency to walk a lot might have been a life-saving choice that will prevent me from losing functions of my legs in significant ways when I’m older. If this whole incident ends up being a small loss of niche mobility as a learning lesson to take care of my knees, it will be worth it. In hindsight, given my odd circumstances and some family history of osteoarthritis, I should have been doing this since forever.
My knee still bothers me sometimes, the episodes seem to be getting milder and rarer, but I doubt I will be able to conclude it has “fully healed” or “failed to heal” until 1 or 2 years from now. I really wish I had a conclusive answer. That this could be a moralistic tale about “the doctors are always right” or “the doctors are dumb” or “do your own investigation and things will work” or whatever. But it isn’t, its a real story about a medical issue, it has a nebulous ending. One that isn’t as horrible as the worst-case scenario, but not a full success by far. Even quantifying how successful I am compared to an average is impossible.
vi - What I’d recommend
If you have a knee injury with a similar diagnostic to mine, I’m sorry. I have almost nothing to recommend to you, the state of medical evidence around this area seems fucked and the prospects for healing are usually bleak no matter what.
I guess I can say exercise that doesn’t cause pain never hurts, so do that. Ideally, find a therapist to help you.
Don’t be hasty in accepting any operation without talking with non-surgeon doctors and figuring out if the literature has any backing for it. Do your risk-benefit analysis, it might be that you can make a decision based on this even with incomplete information.
Take the bog-standard supplements that have a few tiny RCTs and even worse studies showing they kind-of work for reducing pain and improving function for cartilage/tendon/ligament injury and mild to moderate osteoarthritis (collagen peptides, chondroitin, glucosamine, hyaluronic acid, vitamin D3). They likely won’t work but are harmless.
Look into PRP since it’s cheap and has a low rate of complication, consider using it together with restorative surgery (even with bone marrow seeping, which a good surgeon should probably do given current evidence) [14] [15]. It might also serve as a good placebo, depending on how far you think the power of placebo goes.
If you can afford MSCs and can get 2 (ideally 3?) specialists to agree it makes sense in your case (rule of thumb seems to be: somewhat advanced easy to localize injury). Find a clinic that uses bone marrow-derived MSCs rather than bone marrow aspirate directly or fat-derived MSCs. The legality is dubious but they do exist and the best ones seem to use BM MSCs, there is little but strong evidence of them being much better than fat-derived MSCs or aspirate. If you can get treatment from the one Osaka university hospital that ran a study with this, I guess synovial fluid MSCs are even better, but I couldn’t find anyone using them and I tried, a lot.
Finally, one thing I’d recommend that goes against almost all consensus: DON’T USE NSAIDs when you injure your leg. NSAIDs are probably overused in general, and they stop useful processes that may help with healing. But knee injuries seem to be one of the few cases where their toxicity to stem cells and platelets, usually in short supply in the area, may leave you with permanent damage, rather than just delay healing. If it hurts a lot, use opioids. Again, please note, this goes against the consensus and doesn’t have RCT backing.
Overall, it seems like most people agree the goal should be to slowly increase, or at least maintain, your painless range of motion. The healing times also seem long, so I guess being patient might be required.
vii - I am sad
I can’t find reliable data on this (and the irony of this is not lost on me), but somewhere between many dozens of thousands and many hundreds of thousands of meniscus surgeries are performed in the US alone every year. Millions are performed across the world.
Yet the evidence seems to point towards these surgeries being ineffective, mildly harmful in the short run for markers like mobility and pain, significantly in the long run due to accelerating osteoarthrosis. In spite of this, orthopedic surgeons seem unaware and there are no guidelines recommending the avoidance of surgeries.
In my limited reading of what guidelines I could find, all without exceptions recommend a treatment protocol for meniscus injury without citing any evidence about outcomes, let alone thinking about the chance of misdiagnosis or cases where I’d be wiser to wait for better technology or pursue less traditional methods.
I for one am glad I had the scientific literacy, money, patience, and time to navigate the swamp of uncertainty and reach what I think could be a better outcome than the surgery. Alas, I am still far from certain the path I took was correct, but this is a story of navigating, not of setting anchor.
Published on: 2022-12-01